PRIME Annual Report 2019-20
 We are delighted to share our annual report for 2019-20 detailing research and impact highlights from the PRIME Centre Wales team for the past year, including how we have continued to co-produce our research with members of the SUPER patient and public service users group, and our renewed research focus for the forthcoming years. We are delighted to share our annual report for 2019-20 detailing research and impact highlights from the PRIME Centre Wales team for the past year, including how we have continued to co-produce our research with members of the SUPER patient and public service users group, and our renewed research focus for the forthcoming years.


Registration is still open for PRIME Centre Wales' annual meeting, which will be held online, on Tuesday 3rd November, 10:00-15:00. Join us to hear about PRIME's impact, recent efforts to support the response to COVID-19, latest research findings from our network and more. The meeting is free and open to all.
Register your place at: http://tiny.cc/primecentre
|
|
Supporting the response to Covid-19
 PRIME patient safety research response to Covid-19 PRIME patient safety research response to Covid-19
The NHS has and continues to demonstrate impeccable resilience during the pandemic. The service and its professionals have had to adapt and operate under unanticipated circumstances. In peacetime, we know that harm arising from or associated with plans or actions taken during the provision of healthcare, rather than an underlying disease or injury, can be a painful reality for 1 in 20 patients.
With the additional punishing constraints on the system at this time, now more than ever, it is critical that we should be identifying learning from unsafe and substandard care from the first wave in preparation for future insults – from clinicians, managers, leaders, patients and services users; and, more importantly, we should be supporting organisations to use the learning to design processes and systems that keep their patients and themselves safe.
Since lockdown, the Patient Safety work package has sought to be resourceful by collaborating and synergistically exchanging expertise with a diverse range of collaborators (nationally and internationally) to launch multiple patient safety studies. We have closely collaborated with healthcare organisations and embedded researchers into clinical teams tackling COVID-19 to identify essential learning at a critical pace.
Here's a snapshot of some of our studies:
Dr Andrew Carson-Stevens (Patient Safety Work Package Lead) has supported the development of a national incident reporting system for primary care in France alongside researchers at the Université de Nantes. Developed and launched during the height of the first wave of the COVID-19 pandemic, the research team has investigated the nature of unsafe primary care during lockdown using the PISA methods to generate learning from patient safety incidents developed by Dr Carson-Stevens at Cardiff University. The research has been accepted for presentations in November 2020 at the National Congress of CNGE Academic College, France, and the North American Primary Care Research Group Annual Meeting, USA.
During the pandemic, Dr Carson-Stevens was recruited to the UK NIHR Urgent Public Health Review group responsible for the selection, prioritisation, set-up and delivery of studies relating to COVID-19. In Wales, he is a member of the Wales COVID-19 Vaccine Research Delivery Group and is the co-Principal Investigator of the Oxford / Astrazeneca COVID-19 vaccine trial.
Final year Cardiff University medical student, Aniket Paranjape, successfully completed a two-month Wellcome Trust INSPIRE studentship to generate actionable learning from patient safety incidents that occurred between March and July 2020 during the COVID-19 pandemic at a large University Health Board in Wales with his supervisors Dr Andrew Carson-Stevens and Dr Lynette James (Honorary Senior Research Fellow, Patient Safety Research Group, Cardiff University). The research team identified patient safety priorities in terms of where and how the Health Board can strengthen its existing care delivery processes and mitigate avoidable unsafe care to future patients.
Drs Natalie Joseph-Williams (PRIME co-lead for the Person Centred Care Work Package) and Andrew Carson-Stevens, supported by PRIME Research Associate Anna Torrens-Burton and PRIME Research Fellow Dr Alison Cooper, have also sought the patient and service-user perspective of the safety of care received during the lockdown.
The team embedded several patient-reported outcome and experience questions into the COVID-19 UK Public Experiences (COPE) study led by Dr Rhiannon Phillips (Cardiff Metropolitan University). The research team is currently analysing hundreds of responses which offer a unique opportunity to understand unsafe care from the perspective of patients and service users, and will support out efforts to identify where and how health and social care systems can be improved.
Dr Carson-Stevens has also led a multi-disciplinary group of academics from the Business, Engineering, Dental and Medical School at Cardiff University, to investigate health system resilience during the pandemic. In close collaboration with senior leaders and the Emergency Department (ED) at Cardiff and Vale University Health Board, the team are modelling and analysing how performance in complex dynamic socio-technical systems unfolds under varying conditions and are seeking to understand the “mechanisms” behind performance variability. The team has made regular recommendations to leaders responsible for quality improvement and patient safety in the organisation, and they are currently evaluating the introduction of the 'CAV 24/7 appointment system' which is a new and innovative approach to how patients access urgent care during the pandemic.
Several of PRIME's general practitioners (Drs Andrew Carson-Stevens, Alison Cooper, Harry Ahmed and Prof Adrian Edwards) contributed to the Chartered Institute for Ergonomics and Human Factors guidance to support healthcare teams to design work procedures to improve, maintain and sustain resilience.
Alongside our Academic Fellows (Drs Holly Peters and Leigh Sanyalou) based at Cardiff University, and PRIME's Communications & Operations Manager (Mrs Angela Watkins), the team used the guidance to develop a work procedure to detail existing interventions that general practices can use to improve the reliability and safety of triage and call handling processes during the pandemic.
 
 Report on the impact of COVID-19 on sexual behaviour amongst men at risk of HIV in Wales Report on the impact of COVID-19 on sexual behaviour amongst men at risk of HIV in Wales
A team led by Dave Gillespie, Health and Care Research Wales post-doctoral fellow, have recently published a study which provides early insights into sexual behaviour during the COVID-19 lockdown period.
In Wales, people who are at high risk from HIV may be offered medication to substantially reduce their risk of being infected. This is called pre-exposure prophylaxis, or PrEP. The DO-PrEP study aims to understand more about how people in Wales use PrEP, how they access it, and how its use relates to their sexual behaviours.
As part of his research, Dave has been working with sexual health clinics across Health Boards in Wales to recruit men who have sex with men into the DO-PrEP study. Participants have been asked to complete a weekly ‘sex survey’ in which they report the amount of times they have had condomless sex with new or existing partners. Dave was able to analyse the data between 3rd February 2020 and 10th May 2020 in order to assess how the COVID-19 early social distancing measures had impacted the behaviour of PrEP users in Wales.
The research showed that, on average, 42% of participants reported condomless sex in the period prior to the introduction of social distancing measures (16th March 2020) and 20% reported condomless sex after. There was some evidence to suggest that this association was moderated by relationship status. There was a larger reduction in condomless sex in those participants who were single compared to those who were in steady relationships.
The team have shown that the introduction of social distancing measures, and the changes to PrEP services in Wales due to limited access to NHS clinics, was associated with a marked reduction in reported condomless sex among the participants. With the extension of COVID-19 restrictions being extended into the latter part of 2020, and potentially beyond, the team believe that the longer-term impact of social distancing measures on people’s sexual behaviours, and subsequent emotional and mental health, needs closer examination.
See the full report at: Gillespie D, Knapper C, Hughes DA, Couzens Z, Wood F, de Bruin M, Ma R, Jones A, Williams A, Hood K. Early impact of COVID-19 social distancing measures on reported sexual behaviour of HIV pre-exposure prophylaxis users in Wales. BMJ Sexually Transmitted Infections Published Online First: 23 September 2020. doi: 10.1136/sextrans-2020-054598

Wet Age-related Macular Degeneration referral refinement service - impact of Covid-19
Bethan Pugh, Barbara Ryan & Rachel North, School of Optometry & Vision Sciences,
Cardiff University.
The COVID-19 pandemic has severely disrupted eye care services in the UK. In Wales, all routine appointments ceased after March 17th 2020. The Welsh Government and Health Boards streamlined optometric services and it was agreed that patients with emergency conditions such as reduced vision, or those requiring essential care such as spectacle repairs, were to be seen in a reduced number of primary eye care optometric settings by optometrists.
Wet Age-related Macular Degeneration (AMD) is a leading cause of vision loss in people over 60 years of age and as vison loss may be rapid, patients presenting with symptoms require urgent attention. In ABUHB, all patients with suspected wet AMD are referred by optometrists and GPs to an enhanced Macular Degeneration referral refinement service based in an optometric practice in Newport.
During Covid lockdown referrals by optometrist were primarily made from the 16 practices that provided Emergency & Essential care, (however a few other practices remained open to provide services but were not funded by the NHS to do so).
Patients referred to the Macular Degeneration referral refinement centre with suspected wet AMD should be seen within 48hours and the clinical data including scans images of the retina (OCT) are sent to hospital for consultants to triage the patients using a virtual clinic. We commenced an evaluation of the service in January 2020 to determine patient experience of the service and collect clinical data including vision and the time for patients to receive their treatment if needed (intra-vitreal injection). This evaluation continued during the Covid lockdown.
We found a marked reduction in the rate of suspected wet AMD patients being referred to the Macular degeneration referral refinement service during Covid lockdown compared to pre-Covid. During lockdown data suggests that patients were presenting later as they had worse vision, but they were seen more quickly for their treatment. Once lockdown was eased (June 22nd) and routine tests could be provided again by all practices, the rate of referrals increased markedly. The patients referred during Covid were younger than those pre-Covid.
Possible reasons for the reduced referrals could be, that some patients with symptoms of wet AMD are unaware of the urgency for an eye examination and believe that they can wait before seeking attention, or due to fear of contracting the virus by attending the practice, or believing that if they are shielding they can’t seek medical attention. The marked drop in patients attending during lockdown was greater than other reports of reduced attendance for Emergency eye care service (Eye Health Examination Wales) and for Accident & Emergency Departments. All patients who completed a questionnaire stated that the service at the clinic was very good or good. In addition they gave useful feedback to help improve the service.
To conclude, this study suggests that routine sight tests may play an important part in the detection of wet AMD rather than patients presenting as an acute eye problem to an Optometrist. Our recommendations include improving patients awareness of the importance of eye tests for health reasons, especially in older people in order to detect wet AMD; the provision of a leaflet by optometrists that can be given to patients when they are referred into the service, explaining what “referral refinement” is and that no treatment will be given on the day; increasing the number of practices across ABUHB to reduce length of journey for more patients and that consideration should be given to the role of optometrists in reducing the work load of the hospital eye services by being trained appropriately to triage the patients.
The pathfinder evaluation report is now available to read via Cardiff University open access repository.
 How coronavirus highlights the everyday challenges of people with learning disabilities How coronavirus highlights the everyday challenges of people with learning disabilities
Article by Ruth Northway, Professor of Learning Disability Nursing, University of South Wales for The Conversation
Certain groups in society are often labelled as “vulnerable”. If you belong to one of these groups – as an older person, or someone with learning disabilities for example – you may well automatically be considered vulnerable, as though it is an inevitable personal characteristic.
But there are problems with this view, which tends to see vulnerability as a fixed state. Treating it as an inevitable consequence of belonging to a particular group reduces the potential to focus on how vulnerability might be reduced. It also overlooks the fact that we are all vulnerable. Vulnerability is an inevitable consequence of being human.
Indeed, COVID-19 has shown just how vulnerable we all are. Over the course of 2020, we have all had to change how we live our lives, and become vulnerable to loss of freedom, loss of social contact and loss of income. We have also had to deal with real concerns about access to healthcare and our own mortality.
Yet such experiences are everyday life for many people with learning disabilities and their families – and were so, long before the coronavirus emerged.
Read the full article here.
|
|
Other PRIME news of interest
PRIME SUPER group: Service Users for Primary and Emergency care Research

Update from the group
SUPER, the group of public and patient contributors who work with PRIME, are now holding all their meetings online having adapted working practices during the COVID-19 pandemic. At their latest meeting on October 13th, the group heard presentations about three research projects in the following topic areas: Occupational Therapists working in GP clusters; take-up of the flu vaccine by care home workers; paying for social care when the individual has dementia.
The group also held its Annual Meeting. Mari James was confirmed as SUPER chair for a second year. SUPER is preparing to recruit additional new members.
Current online arrangements for meetings may make it easier for people to be involved, without the need to travel. The group will also showcase its work at the forthcoming PRIME Annual Event through oral and poster presentations.
 Recruitment is underway for public contributors to join the SUPER group Recruitment is underway for public contributors to join the SUPER group
We're recruiting, please share this opportunity with anyone who may be interested!
What's involved?
SUPER members provide lay perspectives on developing, conducting and disseminating research about primary and emergency care services. This involvement helps to improve the relevance, quality and dissemination of research on these topics.
SUPER meets quarterly, through meetings in person and online via zoom. At these meetings, researchers and SUPER members discuss research projects which are being developed or are underway. These are the sorts of points which SUPER members make.
- They comment on issues that are important to patients, carers and members of the public.
- They give feedback on the relevance of research topics and how feasible it is to collect information from people.
- They suggest ways of publicising findings from research studies including how to explain complicated or technical messages to non-academic audiences.
- Further information: SUPER group recruitment
Building public involvement and engagement in primary and emergency care research: the story from PRIME Centre Wales
New PRIME publication on public involvement
Policy throughout the United Kingdom promotes involvement of patients and public members in research to benefit patient care and health outcomes. PRIME Centre Wales is a national research centre, developing and coordinating research about primary and emergency care which forms 90% of health service encounters.
In this paper, we describe our approach to public involvement and engagement in PRIME Centre Wales, in particular: how this approach has developed; ways in which public members contribute to PRIME activity; the strengths and limitations of our approach, challenges and future opportunities.
PRIME ensures work is relevant to service users, carers, the public and policy makers by incorporating comprehensive patient and public involvement in every phase of our work.
Bridie A Evans, John Gallanders, Lesley Griffiths, Robert Harris-Mayes, Mari James, Sian Jones, Natalie Joseph-Williams, Mary Nettle, Martin Rolph, Helen Snooks, Carolyn Wallace, Adrian Edwards, and on behalf of the SUPER group and PRIME Centre Wales. Public involvement and engagement in primary and emergency care research: the story from PRIME Centre Wales. Vol 5 No 3 (2020): IJPDS Special Issue: Public Involvement & Engagement.
Read the full article at:
https://ijpds.org/article/view/1363/2617

 Placing patients at the centre of the decision making process in advanced lung cancer Placing patients at the centre of the decision making process in advanced lung cancer
This August saw the publication of the much awaited PACT study by the Marie Curie Palliative Care Research Centre. In this landmark study, researchers followed the journey of patients with advanced lung cancer as they navigated through the process of deciding whether non curative chemotherapy would benefit them or not.
Despite the best intentions, chemotherapy may have serious complications in those with advanced disease increasing the risk of early death, unpleasant side effects and worsening quality of life. Careful planning and discussion is needed in order to make an individualised approach to treatment. Read more.
 Patient and public engagement in medication adherence research Patient and public engagement in medication adherence research
Dr Emily Holmes (pictured opposite) and colleagues from Centre for Health Economics & Medicines Evaluation (CHEME) and Centre for Trials Research (CTR) have worked with members of PRIME's SUPER group to look at ways of improving medication adherence.
Patient and public engagement offers further opportunities to improve medication adherence research. The ABC taxonomy provides a clear definition of “Medication Adherence” for the scientific community, however, interpretation by lay audiences can prove challenging.
The researchers engaged members of the SUPER group (“Service Users for Primary Care and Emergency care Research”), to provide lay perspectives on developing, conducting and disseminating research. During a one-hour meeting held in November 2019, they asked members to comment on: public understanding of the term medication adherence, how best to communicate medication adherence to patients, and how best to involve service users in the design of future studies.
SUPER members agreed that medication adherence was an important topic and suggested future research on an illustrated/animated taxonomy. Discussions focused on the need to adapt terminology for different medicinal forms and potential for subjective interpretation according to experience of acute/chronic and symptomatic/asymptomatic conditions.
Members also encouraged service user involvement throughout the research process and highlighted the need communicate the rationale for improving adherence in addition to explaining the process. The researchers found that the views and experiences of service users provide valuable insight and an opportunity to explore subjectivities that may influence participation and interpretation of medication adherence research.
Findings will be presented by the 24th ESPACOMP, the International Society for Medication Adherence Conference in November.
 Rural WONCA Albuquerque Statement signals a way and a new beginning for rural nursing globally Rural WONCA Albuquerque Statement signals a way and a new beginning for rural nursing globally
Professor Joyce Kenkre, Associate Director of PRIME, has edited a special edition of Journal of Research in Nursing that puts nursing at the forefront of rural healthcare.
“Nurses are an essential element in the delivery of quality primary health care. 48% of the world’s population live in rural areas but only 38% of nurses work there. Nurses need to step up to take a leadership role in rural health, working in partnership with other health care professionals,” said Professor Kenkre.
Nurses have a pivotal role to play as team members in the provision of rural healthcare. This journal edition emphasises the importance of rural nursing care as well as some of the exciting innovations happening around the world. Read more.
 HEAR 2 study new funding HEAR 2 study new funding
Health Experiences of Asylum seekers and Refugees: how well are their interpretation needs met? (HEAR 2)
Dr Gillian Richardson from Public Health Wales in collaboration with Professor Helen Snooks, from PRIME’s emergency, unscheduled and pre-hospital care work package have been awarded funding from Health and Care Research Wales RfPPB programme to investigate the experiences of asylum seekers and refugees with language needs when they seek healthcare within primary and emergency healthcare settings in Wales.
This study builds on the recently completed HEAR study (Health Experiences of Asylum Seekers and Refugees in Wales) which highlighted the need to improve interpretation as a priority within healthcare provision for asylum seekers and refugees.
For further information contact Dr Rabeea’h Aslam on r.w.aslam@swansea.ac.uk
 Congratulations to Professor Stuart Todd Congratulations to Professor Stuart Todd
Congratulations to Stuart Todd, a member of the PRIME team at the University of South Wales on becoming Professor in Intellectual Disability Research. For most of his academic life, Professor Todd has been involved in research with people with learning disabilities and their families and carers, but he has also explored family/carers’ perspectives on caregiving across the life span.
His most recent work focusses on the relationship between death, dying and intellectual disabilities. As well as research, he contributes to nurse education teaching and supervision at undergraduate and postgraduate levels. You can read a profile of Professor Stuart Todd here and see his latest work on the Unit for Development in Intellectual and Developmental Disabilities research website.

PhD success
Congratulations to colleagues, Dr Alison Cooper, PRIME GP Academic Fellow, and Amber Jordan, PRIME supervised postgraduate researcher, Cardiff University, who both successfully defended their PhD thesis in viva (subject to minor corrections).
Alison's research was a realist evaluation of delivering safe primary care in or alongside emergency departments. Alison was supervised by Adrian Edwards, Andy Carson-Stevens and Helen Snooks.
Amber's PhD related to a theory and evidence-based intervention to prepare and support adolescents with long term conditions to participate in shared decision making. Amber was supervised by Fiona Wood, Natalie Joseph-Williams and Adrian Edwards.
Fiona Wood, PRIME co-lead for person-centred care research, and postgraduate research lead at the Division of Population Medicine, Cardiff University, comments:
"We are delighted that these two very able researchers have successfully defended their thesis in viva. Both studies have potential to have impact for the NHS. Both candidates have successfully published from their theses, but it is very gratifying to have a successful result in viva."
 Do you work in community pharmacy or know someone who does and can spare a few minutes to complete our survey? Do you work in community pharmacy or know someone who does and can spare a few minutes to complete our survey?
Our researchers aim to develop UK community pharmacy standards to improve practice for providing palliative and end of life care; we would be extremely grateful if you could follow or share the survey link below:
https://cardiff.onlinesurveys.ac.uk/development-of-daffodil-standards-in-the-context-of-commun-2
Patients experiencing a life-threatening illness require palliative care and access to services to maximise their quality of life. Pharmacy plays a key role in terms of optimising treatment regimens for patients by reducing harm, increasing the value of medication use and improving patients’ and caregivers’ knowledge of medicines.
This can only be achieved by ensuring timely access to palliative medicines as well as effective communication with other healthcare professionals within palliative care teams. In the UK, governmental bodies emphasise the need to engage with stakeholders and focus on the health and well-being of patients, families, and the workforce.
This project, led by Annmarie Nelson (Marie Curie Professor of Supportive and Palliative Care, Scientific Director, & Co-lead for Supportive & Palliative care for PRIME) and Emyr Jones (Consultant Pharmacist) will use an online survey and interviews to investigate community pharmacists’ level of involvement with palliative care patients. This will help identify key priority areas that need to be addressed for ensuring safe, effective, and compassionate services for patient benefit.
If you would like any further information, or have any questions about the study, please contact Dr Anna Torrens-Burton at Torrens-BurtonA@cardiff.ac.uk
 PRIME research at the Health and Care Research Wales annual conference PRIME research at the Health and Care Research Wales annual conference
Members of the PRIME research team were delighted to have the opportunity to take part in this year's Health and Care Research Wales annual conference held 7th October. Our thanks to the organising team for hosting such a well planned and successful meeting, which was held completely online this year.
The conference website offers a chance to view the plenaries, workshops and presentations from the day, with some of the PRIME led contributions listed below:
- Group concept mapping: An interactive consensus method to understand impact in health and social care research. Workshop led by Megan Elliott, Carolyn Wallace and David Pontin, PRIME, University of South Wales.
- Co-design of a logic model describing components. Presentation by Rabeea'h Aslam, PRIME, Swansea University.
- Emergency Admission Risk Prediction (EARP) tools in primary care to reduce emergency admissions to hospital: the gap between evidence and practice. Presentation by Mark Kingston, PRIME, Swansea University.
- Emergency eye care by primary care optometrists providing Eye Health Examinations in Wales (EHEW). Presentation by Rachel North, PRIME, Cardiff University.
- Feasibility of a pharmacy-based referral service for lung cancer symptoms: the PLUS (Pharmacy referral for Lung cancer Symptoms) study. Presentation by Daniella Holland-Hart, Marie Curie Palliative Care Research Centre, Cardiff University.
- Neighbourhood District Nursing. Poster by Sion Tetlow, PRIME, University of South Wales.
- Paramedic supplied ‘Take Home’ Naloxone: a stepped wedge cluster randomised feasibility study. Presentation by Chris Moore, Welsh Ambulances Services Trust.
- Patient-reported Outcome Measures for Rheumatoid Arthritis Symptom Severity. Tim Pickles, Centre for Trials Research, Cardiff University.
- Process Evaluation of the Awareness and Beliefs About Cancer (ABACus). Presentation by Harriet Quinn-Scoggins, PRIME, Cardiff University.
- The Awareness and Beliefs About Cancer (ABACus) trial. Presentation by Kate Brain, PRIME & WCRC, Cardiff University.
- The paramedic will see you now: understanding new roles in primary care. Presentation by Alison Porter, PRIME, Swansea University.
|
|
Recent publications


Mantzourani E, Cannings-John R, Evans A, Ahmed H, Meudell A, Hill I, Williams E, Way C, Hood K, Legay B, Houldcroft L, Deslandes R. Understanding the impact of a new pharmacy sore throat test and treat service on patient experience: A survey study. Research in Social and Administrative Pharmacy. In Press, Available online 10 August 2020.


Kingston M, Griffiths R, Hutchings H, Porter A, Russell I, Snooks H. Emergency admission risk stratification tools in UK primary care: a cross-sectional survey of availability and use. British Journal of General Practice 2020; 70 (699): e740-e748. DOI: https://doi.org/10.3399/bjgp20X712793


Slater D, Hollnagel E, Mackinnon R, Sujan M, Carson-Stevens A, Ross A, Bowie P. A Systems Analysis of the COVID 19 Pandemic Response. Part 1 - The Overview Model. Framsynt. August 2020. https://www.researchgate.net/publication/343944246_A_Systems_Analysis_of_the_COVID_19_Pandemic_Response_Part_1_-The_overall_model


Megan Elliott, Carolyn Wallace, Julie Davies. What methods for evaluating social prescribing work, for which intervention types, for whom, and in what circumstances? A realist review. PROSPERO 2020 CRD42020183065 Available from: https://www.crd.york.ac.uk/prospero/display_record.php?ID=CRD42020183065


Shepherd V, Wood F, Hood K, Griffiths M, Sheehan M. Constructing authentic decisions: proxy decision-making for research involving adults who lack capacity to consent. Journal of Medical Ethics. Sept 2020 (In press) doi: 10.1136/medethics-2019-106042


Poolman M, Makin M, Briggs J, Scofield K, Campkin N, Williams M, Sharma ML, Laird B, Mayland CR. Percutaneous cervical cordotomy for cancer-related pain: national data. BMJ Supportive & Palliative Care 2020. doi: 10.1136/bmjspcare-2019-002057


McCutchan G, Quinn-Scoggins H, Downs T, Ho H, Lam T, Emery J, Weiss B. Psychosocial Influences on Medical Help Seeking for Cancer Symptoms and Treatment in Low- and Middle-Income Countries: A Meta-Analysis and Mixed Methods Systematic Review. JCO Global Oncol 2020:33. DOI: 10.1200/GO.20.28000


Mohd Nor NA, Chadwick BL, Farnell DJJ, Chestnutt IG. 2020. The impact of stopping or reducing the level of fluoride in public water supplies on dental fluorosis: a systematic review. Reviews on Environmental Health 10.1515/reveh-2019-0059
|
|
Events

Registration is still open for PRIME Centre Wales' annual meeting, which will be held online. Join us to hear about PRIME's impact highlights from the last year, recent efforts to support the response to COVID-19, latest research findings from our network and more. The meeting is free and open to all.
Register your place at: http://tiny.cc/primecentre
 Social Prescribing Evaluation Forums Social Prescribing Evaluation Forums
At the Wales School for Social Prescribing Research we will be running three social prescribing evaluation forums per year. The aim of the forums is to provide a place for discussion and resources to support social prescribers and community groups in conducting evaluation and monitoring.
We are inviting members of the Wales Social Prescribing Research Network and the three Welsh Communities of Practice to participate, initially spaces will be limited to 25 people per session and will be allocated on a first come first served basis. We would suggest that 1-2 people per organisation sign up to each session. There will be a waiting list in the event that the forum is oversubscribed.
We will host these forums on Microsoft Teams and joining instructions will be sent to attendees nearer the time.
The dates for the upcoming meetings are:
- Friday 6th November 2020
- Wednesday 20th January 2021
- Tuesday 16th March 2021
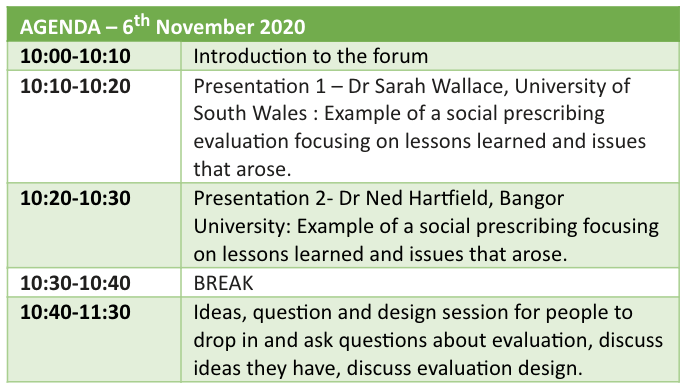
To book a space at the first session being held on 6th November please visit: https://www.eventbrite.co.uk/e/wales-school-for-social-prescribing-research-forum-tickets-124262397175
In addition to the session above we will also be holding three pre-bookable clinic sessions to provide support on specific evaluations. These can be taken up by an individual, or by members from a service/organisation as a group. If you would be interested in booking one of these slots, please complete and return the attached application form to wsspr@southwales.ac.uk.
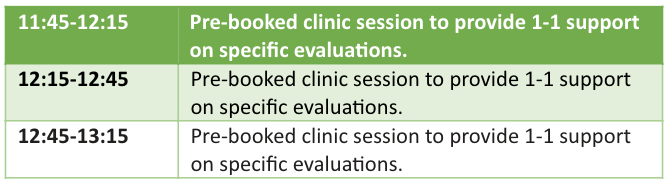
We hope you are able to join us. If you have any queries please don’t hesitate to get in touch by emailing wsspr@southwales.ac.uk
 Changing Healthcare: Learning from lasting change in the NHS Changing Healthcare: Learning from lasting change in the NHS
Dates: 2-6 November 2020
Venue: Online
Join us from 2 to 6 November for this free week-long interactive digital conference. We’ll explore past cases of widespread, lasting change in healthcare and how we can learn from them.
Registration
If you’d like to join any of these events, please register for the conference below and we’ll be in touch with further details.
Registration: https://www.kscopehealth.org.uk/project/changing-healthcare-conference/
 Rural Health and Care Wales Virtual Conference 2020 Rural Health and Care Wales Virtual Conference 2020
Optimising Rural Health and Wellbeing, now and in the future
Date: 10 & 11 November
Booking for this year’s virtual Rural Health and Care Conference is now open, via the following link: https://ruralhealthandcare.wales/rhcw-events/rural-health-and-care-wales-conference-2020/
 Welsh Health Hack Returns! Welsh Health Hack Returns!
Dates:10 & 17 November 2020
The 8th Welsh Health Hack, taking place online on 10 and 17 November. It offers a great opportunity for NHS Staff, universities and industry to collaborate and network to develop early-stage ideas that might solve operational health challenges.
The first stage of the Welsh Health Hack is to request colleagues from Health and Social Care to submit challenges impacting your work.
Find out more and submit your challenge now!
 Multidisciplinary Approaches to AMR: Bench to Bedside and Beyond - free online symposium Multidisciplinary Approaches to AMR: Bench to Bedside and Beyond - free online symposium
Date: Monday 30-Nov-2020 to Friday 04-Dec-2020
We are excited to announce a free online symposium facilitating networking between researchers working across different disciplines with an interest in antimicrobial resistance (AMR).
Organised by GW4 early career researchers, this week-long event aims to address a ‘One Health’ approach to AMR, and will comprise interactive webinars from invited speakers and selected abstracts, themed discussion forums, an online poster session and an ‘Images of Research’ gallery.
Representatives from multiple sectors including academia, industry, human and animal health, environmental science and public policy will be invited to create an accessible, engaging and diverse event. Several broad themes will be covered to explore mechanisms of AMR, novel therapies and technologies, epidemiology, stakeholder engagement and management strategies. This event is open to all researchers with an interest in helping to understand and tackle this global issue.
Registration: https://www.eventbrite.co.uk/e/multidisciplinary-approaches-to-amr-bench-to-bedside-and-beyond-tickets-110982983090
 Genesis Digital 2020 Genesis Digital 2020
Date: 10 December 2020
Time: 09:00 - 18:40
Building on the evolution of the past 19 years, Genesis 2020 will assemble senior executives and decision-makers from across the Life Science, Technology and Investment field to present, discuss and demonstrate their collective insight and thought leadership for the sector, themselves and their stakeholders.

|
|
Funding opportunities
 Social Care Research Fellowship scheme Social Care Research Fellowship scheme
The Fellowship aims to build capacity in health and social care research by supporting individuals to become independent researchers and to undertake high-quality research projects. Applications are invited from individuals working across any sector or scientific discipline to undertake research which will benefit patients, public, service users and/ or carers in Wales.
Applicants will need to demonstrate how their work will benefit service users and carers, and provide training and development opportunities for the proposed fellow. Applicants are expected to show evidence of a clear commitment to a research career and demonstrate how the award will support the potential to become an independent researcher.
Closing date: 8 December 2020
Further information: https://healthandcareresearchwales.org/social-care-research-fellowship-scheme
 RCBC Post Doc Fellowship RCBC Post Doc Fellowship
Applicants must hold registration within the UK as a Nurse, Midwife, Pharmacist or Allied Health Professional (i.e. they must be registered with the NMC, GPC or HCPC upon commencement of study) and reside in Wales for the duration of the fellowship. Biomedical and clinical scientists may be registered with the HCPC or registered through recognised voluntary regulatory arrangements via the Academy for Healthcare Science.
The definition of Allied Health Professions is taken from the Health Professions Council Register and incorporates approximately 15 health professions and 33 protected titles.
Please note that RCBCWales does not have the funding capacity to consider professionals from outside of these healthcare professional groups. Studies will be undertaken through the nursing and allied health departments/schools of our six partner institutions: Bangor, Cardiff, Cardiff Metropolitan, Glyndŵr, Swansea & South Wales Universities.
Deadlines
- Eligible applicants will be requested to submit a full proposal application form by 18th December 2020.
- Eligibility check forms are to be completed and returned to marina.mcdonald@southwales.ac.uk any time up to 13th November 2020
Further information, eligibility check forms and application forms are available at https://www.rcbcwales.org.uk/postdoctoral-funding-opportunities
 Adopting Innovation Adopting Innovation
A programme supporting health care providers to create the conditions that will enable faster and more effective uptake of innovations and improvements.
This programme is open for application until 11 November 2020.
- New programme to build knowledge, skills and confidence within NHS providers to successfully adopt and adapt innovations.
- The Adopting Innovation programme will provide funding for four innovation hubs across the UK with up to £475,000 each for two and a half years.
- Hubs will act as centres of expertise and support within provider organisations to help them, and their local health systems, become better adopters of innovation.
- Expressions of interest are now open until 12.00 (midday) 11 November 2020.
Overcoming the spread challenge – successfully taking up and adapting an innovation in a new setting – is a continuing endeavour for the NHS.
The COVID-19 pandemic is creating unprecedented demands on the health service. Teams are having to rapidly adopt new ways of working and adapt to constant change. As we move into future stages of the response, the NHS will need to continue to innovate to provide patients with the care and support they need.
Through the Adopting Innovation programme, we will support local health systems across the UK in facilitating effective adoption of health care innovations. In doing this, health care organisations can create long-lasting impact for patients and patient care.
Further information:
https://www.health.org.uk/funding-and-partnerships/programmes/adopting-innovation
 RCGP Annual Research Grants RCGP Annual Research Grants
The RCGP Scientific Foundation Board have opened their call for Annual Research Grants. The deadline is 31st July 2019. These are relatively small grants of up to £30,000 but we have had some success with these in the past, particularly from our Academic Fellows.
The SFB is our charitable funding body and awards grants for research projects whose findings will be of direct relevance to the care of patients in the general practice setting. Any GP, primary healthcare professional or university-based researcher may apply for a grant for scientific research to be undertaken in the UK.
Applications for PAGs will be reviewed quarterly according to the following calendar:
- Quarter 4: deadline for submissions 30 November 2020, applications reviewed by 31 December 2020
A maximum of three applications per quarter will be funded.
Further information: https://www.rcgp.org.uk/clinical-and-research/our-programmes/research-facilitation-and-support/research-grants-and-fellowships.aspx
 RCGP support for researchers RCGP support for researchers
The Royal College of General Practitioners (RCGP) is supporting researchers to implement academic primary care findings into practice for GPs.
The Research programme includes:
- Scientific Foundation Board grants
- RCGP Marie Curie Palliative Care Research Fellowship
- RCGP Research Ready®
- RCGP Impact from Research
- Influencing research
- Research awards
The new Impact from Research programme offers to partner on research projects and support impact and dissemination through a range of activities.
Further information: www.rcgp.org.uk/research

NIHR
Health Services and Delivery Research Programme
The commissioned workstream invites applications in response to calls for research on specific questions which have been identified and prioritised for their importance to the NHS and patients. Proposals may include primary research, evidence synthesis, or feasibility and pilot studies. See our current funding opportunities or download a list of potential future research topics currently being developed.
Health Technology Assessment Programme
The Health Technology Assessment (HTA) Programme funds research about the clinical and cost effectiveness and broader impact of healthcare treatments and tests for those who plan, provide or receive care in the NHS.
Public Health Research Programme
The PHR programme invites applications from researchers whose studies will generate new knowledge on the benefits, costs, acceptability and wider impacts of non-NHS interventions intended to improve the health of the public and reduce inequalities in health.
The researcher-led workstream offers researchers the opportunity to submit proposals on topics or research questions within the programme’s remit.
Efficacy and Mechanism Evaluation Programme

Clinical Innovation Hub - Accelerate projects
The Clinical Innovation Hub is a partnership between Cardiff University and Cardiff and Vale University Health Board. The Clinical Innovation Hub is a partner of the Accelerate project, Clinical Innovation Accelerator (CIA). Accelerate is a consortium £24M programme led by the Life Sciences Hub Wales in collaboration with Cardiff University, Swansea University and the University of Wales Trinity Saint David.
It is funded by the Wales European Funding Office (WEFO) and will utilise EU Structural Funds to identify innovation projects that meet an unmet clinical need.
The awards are open to academia, industry, students and healthcare professionals. Innovations could take the form of new technologies, products, processes or services to deliver economically viable solutions for adoption into routine health and social care delivery, for patient benefit, health economic benefit and to stimulate economic growth with attendant socio-economic benefits in Wales.
Support that Accelerate can offer:
- Funding for “Pilot” (6-12 months and <£20K) and “Platform” (12-18 months and < £150K) projects
- Access to future funding opportunities/initiatives
- Clinical input - Buy out and attract in kind NHS staff R&D time
- Human resource - Clinical Innovation fellows, project management, business management, cost benefit analytics and research technologist assistance
- Collaborations - Industry/Academic/Clinical partner
- Advice & Guidance - A Multidisciplinary Team (MDT) of Clinical Innovation experts, including devices and intellectual property experts
- Access to leading Welsh University, University Health Boards and Trusts - patients, facilities and personnel
- Funding /deadlines: Support and awards operate on an always open basis with funding anticipated until 2021 so you can apply at any time. If you would like further information on submitting a proposal or have an innovative idea that you think would benefit from the advice or support for Cardiff University applicants, please contact Barbara Coles: colesb2@cf.ac.uk
Further information:
|
|
|
|